Welcome to the first installment in our 3-part series on measurement-based care in psychedelic therapy, sponsored by Maya Health, an official partner of Third Wave.
Psychedelic therapy may be an uncommon practice, but it’s lightyears away from the fringe. Renowned organizations like Johns Hopkins University and MAPS are leading mainstream conversations through successful psychedelic trials and research programs. Simultaneously, legal ketamine clinics are actively treating depressed patients across the country. The ‘heal thyself’ renaissance is underway, yet its future is still uncertain.
Research success doesn’t always align with practice results. That gap in outcomes, along with psychedelic misconceptions, could interfere with widespread acceptance. To convince the masses that psychedelic therapy is a mental-health innovation worth championing, clinicians must hold space for a data-driven treatment model.
Why Psychedelic Therapists Need Measurement-Based Care
Psychedelic therapy is undoubtedly the most promising new protocol for anxiety, depression, and PTSD, among other mental health issues. Still, psychedelics are not a panacea. They don’t come wrapped in a standardized happiness package that works the same for everyone. Psychedelic therapist support is nearly just as crucial as plant medicine itself. That’s why ketamine clinicians, integration coaches, and even retreat facilitators need highly effective tools and strategies to create personalized plans for individual self-healing.
Measurement-based care (MBC) is a tool that helps clinicians use validated symptom-rating scales to make better decisions for their patients compared to standard note-taking models. MBC generally incorporates digital tools that help therapists measure progress and track decisions about dosing and frequency. Research shows MBC also allows clinicians to learn from real-time feedback following sessions and revise plans if the patients aren’t responding–or worse, are deteriorating.
This highly efficient feedback loop, called “progress monitoring” or “outcome monitoring”, is critical to advancing psychedelic therapy, improving quality of care, and relieving suffering worldwide.
Just the facts
- Patients sometimes feel worse during the course of psychiatric treatment. The MBC feedback system helps reduce their chances of symptom deterioration.
- MBC helps reduce psychological distress and interpersonal issues while improving quality of life and social functioning–especially for patients defined as “treatment-resistant”.
- Most randomized controlled trials with frequent and timely feedback on patient-reported symptoms display significantly improved outcomes than the standard model.
- Patients whose therapists reviewed the self-report Behavior and Symptom Identification Scale with them in-session said they felt a greater sense of involvement in decisions than clients without self-report symptom monitoring.
- Patients who completed self-reports of depressive symptoms said the assessment allowed them to quantify their symptoms and better understand their experience with depression.
Psychedelic therapists need MBC to know what does and doesn’t work, and their patients need to be empowered during the process. Through this data-driven and patient-centered approach, psychedelic therapists and integration coaches can develop more informed treatment methodologies and demonstrate the safety and efficacy of their practices.
Yet Measurement-Based Insight is Missing (for now)
“Outside of note writing, much of psychiatric evaluation is subjective and takes place in the examiner’s brain.” – Daniel Barron, Reading Our Minds: The Rise of Big Data Psychiatry
Note-taking is the norm among therapists, but this approach makes it difficult to measure outcomes and adjust treatment protocols in real time. Still, we’re not blaming the field of psychology for this approach. Until recent years, therapists had no choice but to rely on outdated, self-reported assessments like the Diagnostic & Statistical Manual of Mental Disorders (DSM) and questionnaires like the PHQ-9 to diagnose and treat patients manually.
Fortunately, 21st-century advancements like electronic health records, health information technology, and the Standard for Clinician’s Interview in Psychiatry (SCIP) offer alternatives that support informed (and quicker) decisions in real time. But not all therapists are ready to make the jump. Many therapists believe measurement-based scales are clinically ineffective, while others worry the technology is too difficult or expensive to implement. As a result, only 18% of psychiatrists and 11% of psychologists use symptom-rating scales regularly in their approach. More than 80% continue to manually record diagnoses, symptoms, and treatment in an undefined narrative, making it difficult to measure or compare outcomes of patients that different clinicians have assessed.
Why Now Is the Perfect Time to Start Measuring
The loose-outline model is obsolete, and now is the perfect time for an update. Advances in health information technology, remote monitoring via mobile devices, and web-based training make it simple for therapists to implement measurement-based care in their psychedelic practices. The setup cost is minimal, and the benefits are measurable. Additionally, as the field of psychedelic medicine becomes more commonplace, accreditation organizations may require clinics to implement MBC in their practice.
Why? Psychedelic therapy is a highly nuanced treatment type involving altered states of consciousness. So required or not, therapists may be well advised to consider documenting their patients’ diverse mind-opening journeys, including measuring baselines, preparation strategies, integration plans, and everything in between. The psychedelic community can overcome political and social skepticism. But this can be overcome with enough data providing evidence for the safe and effective practices existing across the ecosystem.
How Psychedelic Therapists Can Implement MBC Now
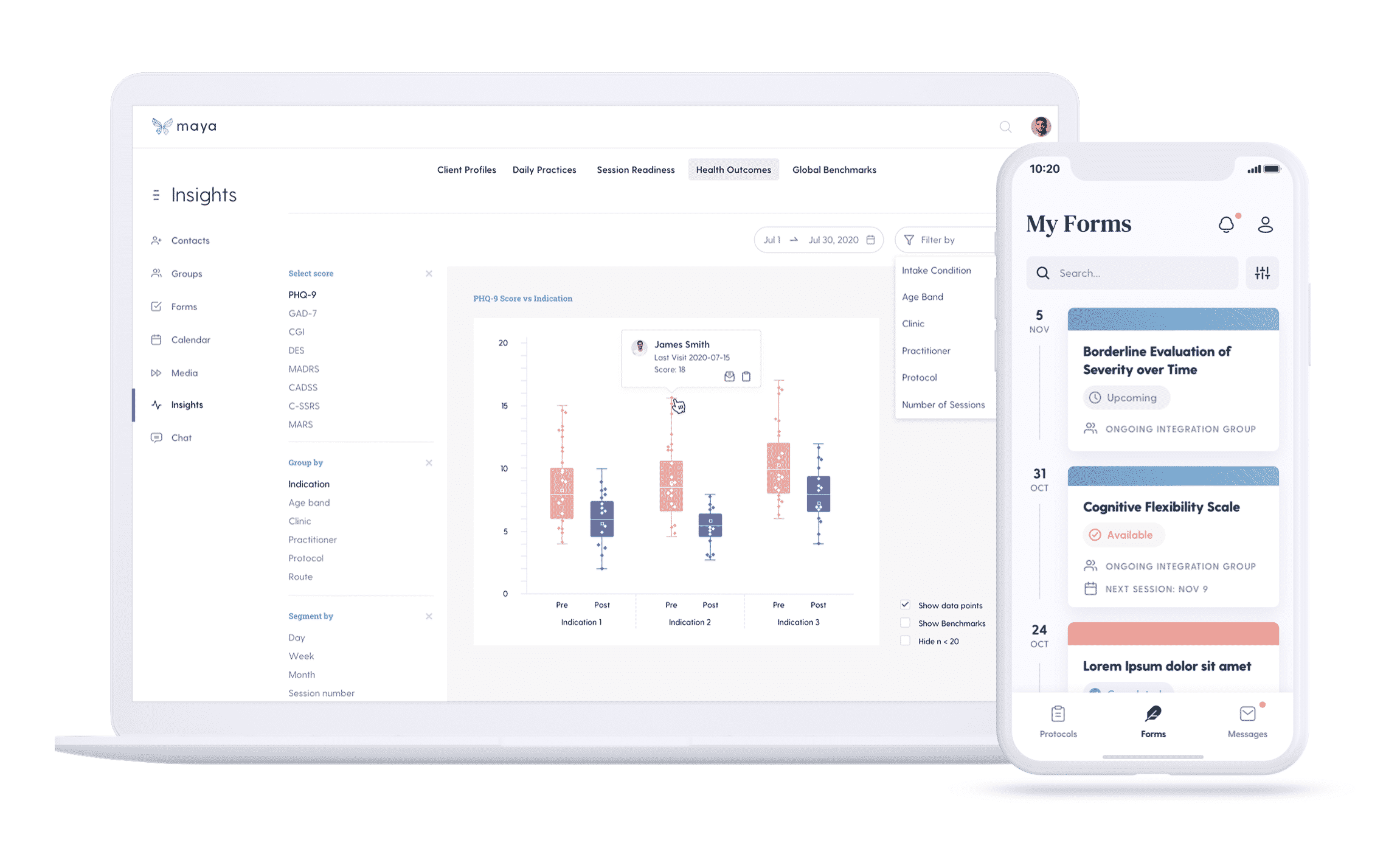
MBC helps save time and increase efficiency while elevating psychedelic clinics and patients to greater wellness. Fortunately, digital platforms like Maya exist to support psychedelic therapists, integration coaches, and retreat leaders to guide more meaningful journeys. Over the past two years, the Denver-based Maya team has been gathering feedback from psychiatrists, psychologists, psychedelic therapists, and retreat leaders worldwide to guide the creation of the platform. As a result, Maya allows practitioners to quickly implement measurement-based care in a purposeful way that saves time on routine tasks and strengthens communication with their patients.
Platforms like Maya empower Psychedelic therapists to:
- Collect baseline measurements about health, wellbeing, and lifestyle
- Streamline intake and preparation
- Measure and visualize therapeutic progression
- Create treatment protocols and save templates for automation
- Communicate via HIPAA-compliant, encrypted chat
- Follow up with clients to support integration
- Join a global learning community of practitioners
- Contribute aggregated data to the field of psychedelic research
The Bottom Line
Using data gathered from other providers worldwide, psychedelic therapists and coaches can begin to close the gap between clinical research and real-world practice. They can also treat patients more mindfully and methodically, supporting people with greater efficiency on their journey to physical, mental, and emotional wellbeing.
If you are curious about implementing MBC in your practice, we encourage you to explore Maya as a platform to help with a seamless transition. Maya is offering practitioners and clinics 20% off and exclusive access to the platform before it’s available to the public. To redeem the limited-time offer, mention ThirdWave in “referrals” when you sign up.
For a complete list of trusted ketamine-assisted psychedelic therapists, visit Third Wave’s Psychedelic Directory.







