
Disclaimer: This article is not medical advice. If you’re considering microdosing to help with symptoms of depression or to help wean off SSRIs, consult a physician or medical professional first.
Additionally, psychedelics are largely illegal substances, and we do not encourage or condone their use where it is against the law. However, we accept that illicit drug use occurs and believe that offering responsible harm reduction information is imperative to keeping people safe.
Microdosing has become increasingly common since James Fadiman, Ph.D. popularized the practice in his 2011 book, The Psychedelic Explorer’s Guide. In the Global Drug Survey ten years later, one in four people who used psychedelics also reported microdosing for mental health benefits like alleviating depression symptoms. Many people discontinued antidepressant medications as a result.
Today, more and more people are microdosing or taking low, sub-hallucinogenic psychedelic doses for mental health and reevaluating their relationships with pharmaceuticals like Prozac, Zoloft, and Lexapro.
Watch the video above highlighting the critical differences between microdosing classic psychedelics and antidepressants for treatment-resistant depression and anxiety. Read on for a comprehensive overview of recent psychedelic research comparing microdosing to antidepressants in clinical and real-world settings.
Antidepressants: Efficacy and Mechanism of Action

Patients have been using pharmaceutical antidepressants, like selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and monoamine oxidase inhibitors (MAOIs) since the first MAOI in the 1950s.
SSRIs are the most common antidepressant medications in modern psychiatry. Known as antagonist antidepressants, SSRIs increase serotonin levels by activating the brain’s 5-HT1A receptors and inhibiting the 5-HT2A receptors.
SSRIs’ serotonin action purportedly treats depression and anxiety by improving mood, enhancing positive emotions, and improving sleep. However, longitudinal research indicates selective serotonin reuptake inhibitors have serious limitations.
A systematic review of 232 double-blind placebo-controlled trials revealed that antidepressants are more effective than placebo, but the difference is minimal statistically speaking. Antidepressants only provide limited benefits to a small population subset.
Of 73,000 patients reviewed, less than a quarter experienced significant symptom relief. Of those patients, just 15% showed benefits beyond a placebo effect. Interestingly, the study focused on near-term efficacy and didn’t identify long-term trends.
A 2022 panel survey analysis published in PLOS One analyzed patients over 11 years. The study determined that patients on antidepressants didn’t experience improved quality of life compared to those not on SSRI-type medications.
MAOIs and SNRIs claim to be more effective than SSRIs because they increase levels of serotonin and other neurotransmitters.
- SNRIs increase norepinephrine levels, which are associated with energy and attention.
- MAOIs increase serotonin, norepinephrine, and dopamine, which can improve mood and reduce panic.
Still, research indicates SNRIs are no more effective than traditional SSRIs for treating anxiety disorders. And MAOIs have significant side effects beyond the standard sleepiness, nausea, and diarrhea that many antidepressant patients report. MAOIs can also cause blood pressure spikes and seizures when mixed with common foods like chocolate, aged cheeses, processed meat, and red wine.
How Psychedelics Act Differently

Antidepressants’ lackluster results may be due to the neuroscience of how SSRIs and SNRIs act on the brain, compared to psychedelics. Both drugs interact with the body’s serotonin system, but in distinct ways.
Traditional psychedelic compounds bind with postsynaptic serotonin receptors known as 5-HT1A, while classic psychedelics primarily act on 5-HT2A receptors.
Renowned psychedelics researcher Robin Carhart-Harris published a notable paper on this topic, illustrating why antidepressants’ and psychedelics’ receptor preferences matter to mental health outcomes.
According to Carhart-Harris, serotonin neurotransmission correlates to “two distinct adaptive responses to adversity.” 5-HT1A agonists like Prozac lead to “passive coping,” while 5-HT2AR activation mediates “active coping.”
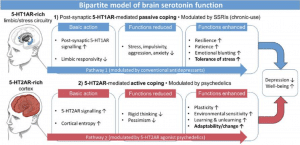
Photo credit: Serotonin and brain function: a tale of two receptors
In other words, antidepressants dampen emotional intensity, reducing the mental and physical sensations associated with stress, depression, and anxiety.
Such numbing effects can be profoundly beneficial, especially for those who feel suicidal. But SSRIs’ 5-HT1A affinity may also lead to emotional repression, compartmentalization, and lack of motivation, ultimately making people emotionally stunted, less resilient, and less patient when faced with challenges. In some cases, antidepressants can cause or exacerbate anhedonia, a condition where life feels gray and bleak.
Classic psychedelics, like LSD and psilocybin, act on various neurotransmitters, including serotonin, dopamine, glutamate, and adrenergic. Most research, however, focuses on LSD and psilocybin’s strong affinity for particular serotonin channels.
Acting on 5-HT2A and 5-HT2C receptors, these traditional hallucinogenic compounds quiet brain regions associated with mind-wandering, fear, and hypervigilance while activating networks responsible for visual input, higher learning, memory, planning, goal-setting, and instinct regulation.
Psychedelics’ ability to reorganize the brain’s ordinary communication networks through neuroplasticity brings people face to face with the root causes of their depression and anxiety, typically with less judgment and distress.
In the process, psychedelics promote catharsis, an emotional release, and meaning-making, allowing people to reframe traumas into stories with transformative lessons. “Active coping” helps free people from clinical pathologies like treatment-resistant depression by confronting rather than avoiding discomfort.
The Benefits of Psychedelics vs. Antidepressants
Psychedelics also exhibit several functional benefits over antidepressants:
- Fast results:
Antidepressants can take four to eight weeks before kicking in. Conversely, psychedelic effects occur in about an hour and provide rapid relief. Sometimes, just two psilocybin doses can free people from depression for at least a year. - Fewer Side Effects:
No drug is without side effects, but psychedelic-related side effects are typically mild and short-lived and include increased breathing rate, loss of appetite, uncoordinated movement, and sleep issues. Rare yet serious risks like prolonged psychosis occur. But medical professionals can screen patients to avoid these occurrences.
On the other hand, antidepressant side effects are widespread as the body adjusts to the medication and can be persistent, including:
- Weight gain
- Sexual dysfunction
- Weakness
- High blood pressure
- Stomach issues
- Insomnia
- Nervousness
- Drowsiness
- Seizures
- Less Frequent Use:
Rather than a daily pill, psychedelics can be a one-time or infrequent treatment option that provides long-term effects. High-dose psychonauts may only need a couple of sessions. Microdosers take one to five doses per week, interspersed with extended periods with no consumption.
High-Dose Psychedelics Depression Research
The breadth of clinical research today focuses on high-dose psychedelic experiences, including the following three studies:
1. A 2021 phase 2 double-blind randomized controlled trial that compared psilocybin with escitalopram (an SSRI) for severe major depressive disorder.
Results:
The psilocybin and escitalopram groups both improved from baseline without significant differences from one population to the other. However, psychedelic patients achieved much higher remission rates, 57%, compared to 28% on escitalopram.
2. A randomized, double-blind trial led by Roland R Griffiths and Matthew W Johnson of Johns Hopkins analyzed 51 patients with untreatable cancer diagnoses, comparing a placebo to a high-dose psychedelics group.
Results:
Clinician- and self-rated measures of depression, mood and anxiety, quality of life, meaning, optimism, and death anxiety improved significantly in the high-dose psilocybin therapy group. Notably, 80% also exhibited clinically significant improvements in the six-month follow-up.
3. Recently, a mental health company, COMPASS Pathways, concluded a phase IIb clinical trial investigating psychedelic therapy for treatment-resistant depression
Results:
36.7% showed significant improvements after three weeks, and nearly 30% achieved total remission. Patients who received the 25 mg dose demonstrated the most statistically substantial symptom reduction with a “rapid and durable” treatment response.
As the above research shows, high psychedelic doses combined with psychotherapy support appear to be the most effective protocol for rapidly reducing depression symptoms and achieving clinical remission.
At the same time, mind-blasting hallucinogenic experiences might not suit everyone. Radically altered states of consciousness can bring up triggering material that not everyone is prepared to handle.
Rather than jumping into the deep end, many are looking at microdosing psychedelics to take that first step, reporting positive and enduring mental health benefits that antidepressants have failed to provide.
Microdosing vs Antidepressants: What Does the Research Say?

Microdosing doesn’t have the same volume of clinical research as macrodosing. However, prominent institutions and experts are changing that through clinical studies and citizen questionnaires.
James Fadiman, called the “father of microdosing,” began collecting anecdotes from hundreds of self-reported microdosers in 2010. A year later, Fadiman published The Psychedelic Explorer’s Guide, outlining sub-perceptual benefits like heightened well-being and improved focus.
Notably, Fadiman explained microdosing’s key advantage over high-dose experiences; people can incorporate low doses into daily life without risk or inconvenience. Microdosers don’t need the perfect mindset or physical environment. And they don’t need a therapist onsite or a dedicated day off. People can experience small doses of psychedelics’ mental health benefits and continue functioning normally.
In 2019, Fadiman and researcher Sophia Korb, Ph.D. published the first worldwide, open-enrollment exploratory microdosing study with results from more than 1,000 people across 12 countries over 18 months. Many participants followed the Fadiman protocol of one day on and two days off for at least the first month.
After the survey period ended, microdosers reported:
- Improvements in negative moods, especially depression, for longer than 14 days
- Increases in positive moods
- More energy and work effectiveness
- Improved health habits
Further Research on Microdosing vs Antidepressants
Since Fadiman and Korb’s exploratory study, more microdosing psychedelics research has emerged:
- A 2021 international survey of 8,703 people from 84 countries revealed a connection between microdosing and reduced symptoms of depression, anxiety, and stress. Microdosers most commonly used psilocybin (85%) at various doses and protocols. Many reportedly followed the Stamets Stack method, including Lion’s Mane mushrooms, chocolate, and niacin. Participants with mental health concerns showed lower levels of depression, anxiety, and stress across genders.
- A 2022 study analyzing LSD microdosing’s neural action versus placebo and behavioral changes found LSD dose-dependently increased positive mood, joy, and energy and reduced anxiety. Microdosing also slightly altered consciousness into what was described as a “blissful state” without any hallucinogenic or other sensory changes.
- In 2022, famed mycologist Paul Stamets, Pamela Kryskol MD, and a Canadian research team published an observational study comparing 953 microdosers to 180 non-microdosers across one month. Among its findings, the study revealed that most people with moderate depression at the baseline assessment reported an improvement to mild symptoms after 30 days of microdosing.
- In 2022, the University of Chicago researchers published a laboratory-controlled microdosing study with results that failed to reflect most survey findings. The study included two microdosing groups, taking either 13 or 26 micrograms of LSD, and a placebo group. After the first session, the 26-microgram participants experienced increased stimulation and decreased negative mood during a task miming social rejection. However, these effects waned throughout the sessions. Additionally, the 13-microgram dose group didn’t experience any noticeable changes.
Self-reported, observational research on microdosing versus antidepressants for anxiety and depression exhibits promising results. But in-laboratory, placebo-controlled experiments have failed to replicate these outcomes. Some suspect this dissonance may be due to the placebo effect, where microdosers feel better due to their expectations rather than the substance itself.
Some truth may exist in that suspicion. But psychedelics experts and researchers argue that lab-based studies can’t possibly mimic microdosing’s real-life mental health benefits. Researcher Suresh Muthukumaraswamy, Ph.D., articulated this in a recent Third Wave podcast:
I think the set and setting … applies to microdosing. There’s a clear difference in our data between a dose taken in a laboratory and a dose taken out in the wild as people do daily activities. I think that’s why those other studies haven’t replicated what the community is reporting because they’re doing it in a boring laboratory.
Microdosing research has a long way to go before anyone can understand the precise pharmacology or compare low-dose psychedelics to antidepressant effects.
Still, self-reported surveys indicate the practice is well tolerated and often transformative. People with mental health concerns who feel called to microdose LSD or psilocybin should work with their doctor or therapist to determine an appropriate protocol.
Interested in microdosing to support your healing and growth? Get Third Wave’s Microdosing Course which gives you the essential information to begin a mindful microdosing practice.
Is it Safe to Microdose While on Antidepressants?
Many think they need to wean off antidepressants before trying psychedelics due to potential risks like serotonin syndrome. That risk is real with some psychedelic drugs, like MDMA and ayahuasca.
Psilocybin and LSD, however, are classic tryptamines, meaning they only partially stimulate serotonin receptors and do not interact with the same neural pathways as SSRIs and SNRIs. People who combine classic psychedelics with antidepressants should not experience adverse physical reactions in most cases.
Anecdotally, Global Drug Survey respondents corroborate this message. Several microdosers reported simultaneously taking antidepressants without side effects, and almost half reduced or stopped antidepressant usage as a result. Additionally, a double-blind, placebo-controlled study indicated that psilocybin and SSRIs together did not negatively interact in the body.
However, to get the best outcomes, antidepressant patients may have to experiment to find the right micro-dosage. In a recent Third Wave video, Paul F. Austin explained that people on SSRIs typically need a higher-than-average microdose amount. In contrast, SNRI patients might need lower-than-average doses to achieve that Goldilocks effect.
Regardless, safety is not guaranteed.
All those considering adding psychedelic microdoses to their mental health regime must do so with a medical professional, preferably a psychedelic-informed psychotherapist.
Looking for a reputable practitioner for your own microdosing or psychedelic medicine experience? Check out Third Wave’s psychedelic directory. You’ll find a carefully curated list of high-quality, vetted providers you can trust.
Should I start with Psilocybin Mushrooms or LSD for Microdosing vs Antidepressants?

People can theoretically microdose any psychedelic substance, like ketamine, MDMA, and DMT. However, most microdosers utilize LSD or psilocybin.
LSD and psilocybin microdosing experiences are noticeably different, so first-timers should consider their goals and desired effects when choosing their desired substance.
When deciding between LSD vs. psilocybin to microdose versus antidepressants, Third Wave founder Paul F. Austin recommends psilocybin for the initial protocol. Psilocybin comes from magic mushrooms, an organic compound many prefer when weaning off synthetic antidepressants. The effects of psilocybin can also effectively connect people to their present-moment emotions and typically feel less stimulating than LSD.
What’s the Best Mushroom Microdosing Protocol?
According to Paul F. Austin, most ‘microdosers’ use about 10% of the regular dose of psilocybin, equivalent to about 100-300 milligrams of dried mushrooms. Typically people consume mushroom microdoses between two and five times a week.
If you’re interested in growing your psilocybin mushrooms at home, check out Third Wave’s Mushroom Grow Kit and Course. Excluding mushroom spores, this kit provides everything you need to cultivate your own renewable microdosing supply.
Final Thoughts on Microdosing versus Antidepressants
Anecdotal reports and observational studies suggest that microdosing psychedelics can improve learning, enhance mood, and reduce symptoms of anxiety and depression. Most studies do not include control groups or longitudinal data, so scientists must continue exploring the practice before anyone can reliably compare the practice to antidepressants.
People drawn to microdosing should seek guidance from doctors and psychedelic-informed mental health professionals. Sub-hallucinogenic psychedelic doses can offer a valuable, heart-opening alternative to antidepressants, which have left many frustrated, detached, and desensitized.
Visit Third Wave’s psychedelic directory to find high-quality, vetted therapists to help guide your mental health journey.







