Disclaimer: Psychedelics are largely illegal substances, and we do not encourage or condone their use where it is against the law. However, we accept that illicit drug use occurs and believe that offering responsible harm reduction information is imperative to keeping people safe. For that reason, this document is designed to enhance the safety of those who decide to use these substances.
This article has been medically reviewed by Katrina Oliveros, MSN-ED, BSN
Nervous system dysregulation has emerged as a silent epidemic drastically impacting mental and physical well-being.
This deeply imbalanced state urgently needs more research, compassion, and novel healing practices to address its widespread impact. Once shrouded in stigma, psychedelics reveal themselves as a beacon of hope.
This article explores the intersection of psychedelics and mental health, shedding light on their potential to recalibrate a dysregulated nervous system and restore internal peace.
The Nervous System and Dysregulation
The nervous system is a complex network of nerves and cells that transmits signals between different body parts. The nervous system regulates critical functions and the body’s response to internal and external stimuli.
When the nervous system functions well, humans can more easily adapt to the world’s ever-changing environment. However, a dysfunctional nervous system immediately interferes with the body’s ability to respond to and recover from stressful situations.
Understanding the Nervous System
The nervous system consists of two principal, symbiotic parts: the central nervous system (CNS) and the peripheral nervous system (PNS).
The CNS includes the brain and spinal cord and acts as the body’s command center.The CNS receives information from sensory receptors, processes that data, and sends instructions to the rest of the body through the peripheral nervous system.
The PNS, a set of nerves branching off the spinal cord, receives and transmits CNS commands to limbs and organs, governing everything from heartbeat to walking.
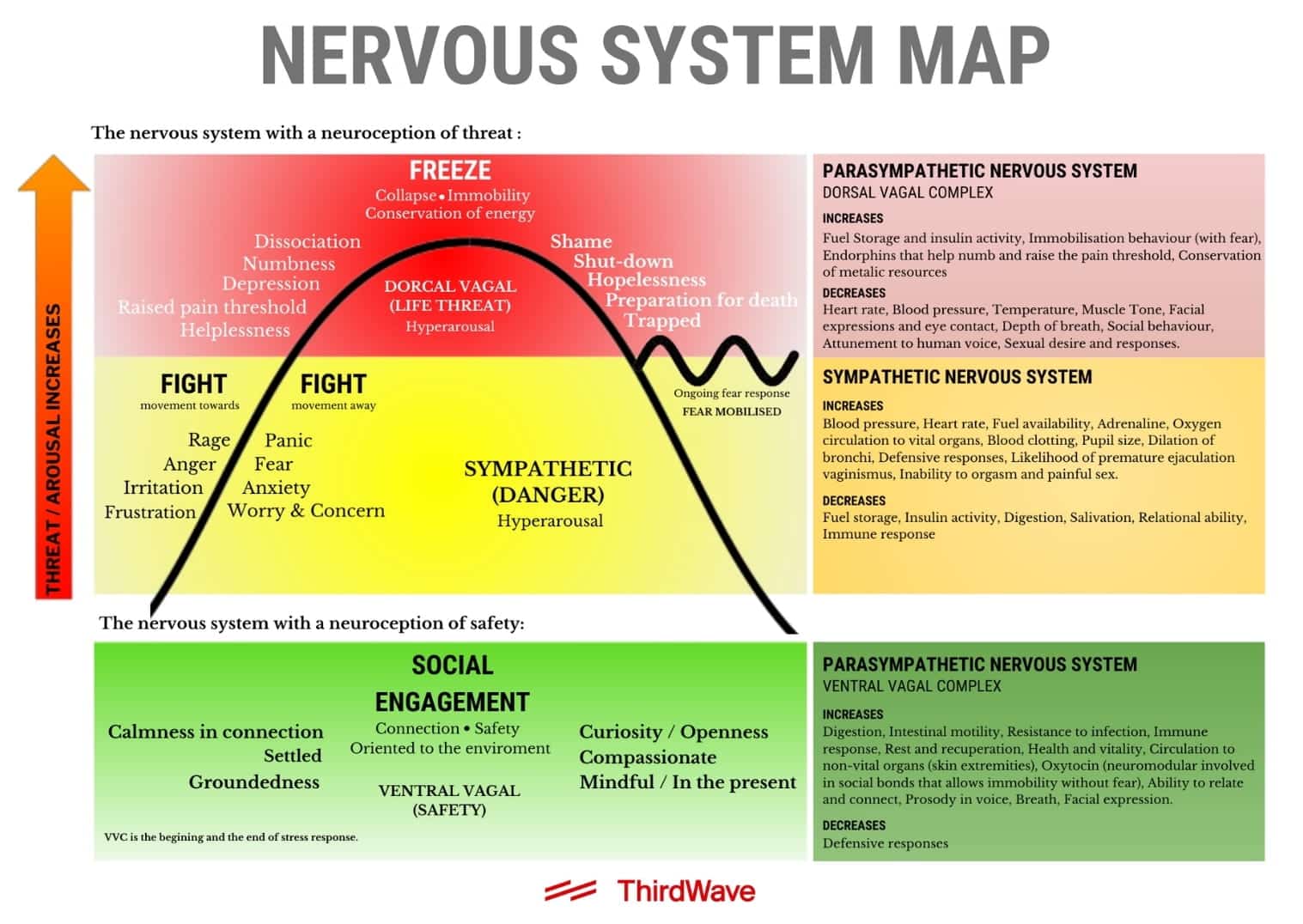
Within the peripheral nervous system lies the autonomic nervous system (ANS), a nerve network that controls unconscious processes, like breathing, which are critical to survival. The ANS further divides into the sympathetic and parasympathetic autonomic nervous systems, which work in opposite ways to regulate different body parts.
- The sympathetic autonomic nervous system (SANS) controls the body’s physiological response to stress, known as “fight or flight.” SANS activation causes the body to release a flood of stress hormones like adrenaline and cortisol in response to a real or perceived threat
- The parasympathetic autonomic nervous system (PANS), associated with the vagus nerve, helps the body conserve energy in a state known as “rest and digest.” Parasympathetic activation causes the heart rate and blood pressure to decrease, while promoting blood flow to digestive organs.
The peripheral nervous system also houses the somatic nervous system (SNS). This subdivision controls voluntary muscle movements and sensory information processing. The SNS plays a crucial role in actions like walking, talking, and grasping. Its neurons also send information from the skin and muscles back to the brain, allowing people to perceive touch, temperature, and pain.
The limbic system, a collection of interconnected brain structures, is deeply tied to nervous system networks. The limbic system registers emotional responses and links them with cognitive functions and physiological actions, like motivation, learning, memory, and hormone release.
When the limbic system registers fear or excitement, the sympathetic nervous system activates its “fight or flight” stress response. Conversely, limbic-resonated relaxation can engage the parasympathetic nervous system to rest and digest.
Curious about exciting opportunities as a psychedelic practitioner?
Curious about exciting opportunities as a psychedelic
practitioner?
practitioner?
Our FREE E-Book, "Top 3 Emerging Psychedelic Careers," offers a guide to navigating the psychedelic industry.
Plus, you'll receive an exclusive webinar where you can dive deeper and explore these potential career paths.
Causes and Signs of a Dysregulated Nervous System
The nervous system enables a coordinated and adaptable interface with the world. However, everyday stressors and health conditions can quickly and dangerously disrupt this balance.
A dysregulated nervous system can overstimulate the sympathetic response and under-activate the parasympathetic response, creating a constant onslaught of stress hormones while inhibiting the body’s ability to recalibrate.
1. Common Causes of Dysregulation:
- Traumatic Events: Exposure to traumatic events, including physical or emotional abuse, can disrupt the nervous system’s ability to regulate itself. Anxiety, anger, agitation, fear, and hyperactivity can all result from remaining in this state.
- Chronic Stressors: Continuous exposure to stressors like job dissatisfaction, financial difficulties, and relational challenges can keep the body on high alert, leading to overreacting to even minor triggers.
- Health Conditions: Certain underlying health conditions, such as hormone imbalances, autoimmune disorders, chronic inflammation, autism, and ADHD, can disrupt the delicate balance of the nervous system.
2. Signs and Symptoms of a Dysregulated Nervous System:
- Heart Rate and Blood Pressure: People with nervous system dysfunction commonly experience fluctuations in heart rate and blood pressure, reflecting the body’s erratic response to stressors.
- Sleep Disturbances: Difficulty falling or staying asleep is a common symptom, as an imbalanced body remains on high alert even during rest.
- Heart Rate Variability: Reduced heart-rate variability indicates a lack of adaptability in the autonomic nervous system, a sign of dysregulation.
- Dissociation: Nervous system imbalances can cause dissociation, a common issue linked to trauma. Dissociation refers to a detachment from reality or self.
- Chronic Pain: A dysregulated nervous system can lead to persistent pain as the body’s standard pain-regulation mechanisms become disrupted.
- Overreacting: An exaggerated response to minor stressors is a common sign of underlying dysregulation.
Effects of Dysregulation on Physical & Mental Health
A dysregulated nervous system can significantly impair mental health by disrupting the body’s natural balance between stress and relaxation.
A constant state of high alert can also strain the immune system and physical body, causing or exacerbating chronic conditions related to heart rate, blood pressure, and pain. Sleep disturbances further aggravate physical and mental health issues.
1. Physical health issues
- Cardiovascular stress from irregular heart rates.
- Heart disease from uncontrolled high or low blood pressure.
- Insomnia from chronic sleep disruption.
- Muscle and joint pain from chronic tension and inflammation. .
- Metabolic disorders like weight gain and obesity from lack of rest and digestion resources.
- Skin conditions, like eczema and psoriasis, are exacerbated by stress.
- Migraines and headaches from chronic tension.
- Chronic fatigue or general energy depletion from a frequent high alert state.
2. Mental Health issues
- Anxiety Disorders: Including generalized anxiety disorder and panic attacks.
- Depression: Chronic feelings of sadness, hopelessness, and lack of motivation.
- Post-Traumatic Stress Disorder (PTSD): Re-experiencing trauma through flashbacks and nightmares.
- Emotional Dysregulation: Difficulty in managing and responding to emotional stimuli appropriately.
- Relationship Difficulties: Struggles with interpersonal relationships due to overreacting or emotional detachment.
- Obsessive-Compulsive Disorder (OCD): Persistent, unwanted thoughts exacerbated by stress and anxiety.
- Eating Disorders: Such as anorexia or bulimia, potentially linked to stress and emotional dysregulation.
- Substance Abuse Disorders: Over-using substances to cope with emotional and mental strain.
Nervous system dysregulation is challenging to resolve due to complex adverse effects, individual variability, and interconnectedness with other bodily systems. Resolving the imbalance requires a comprehensive, individualized approach.
Psychedelics and Their Potential to Heal a Dysregulated Nervous System
Psychedelics present a multifaceted tool for healing a dysregulated nervous system. They have long been part of cultural traditions and therapeutic practices, and now, the scientific community recognizes their potential to regulate a dysregulated nervous system.
What are Psychedelics?
Psychedelics, often referred to as “entheogens” in the context of spiritual practices, are compounds that induce altered states of consciousness.
They include substances like LSD, psilocybin (found in magic mushrooms), and DMT (found in ayahuasca). These classic psychedelic compounds activate serotonin receptors throughout the brain and nervous system, regulating how one processes and responds to emotional and sensory inputs.
The resulting experience induces profound changes in perception, emotion, and thought patterns. Visual and auditory hallucinations are also common, accompanied by a distorted sense of time and space.
Some also report spiritual or mystical experiences, including deep insights into themselves or the universe and a sense of interconnectedness with nature or other beings.
Historical and Cultural Use of Psychedelics for Healing
Various indigenous cultures have employed psychedelics in healing and spiritual ceremonies.
For example, the Native American Church ingested peyote in sacred ceremonies to promote emotional and psychological healing. In the Amazon Basin, shamans have used ayahuasca as a medicine for physical and spiritual ailments for centuries. The Mazatec people of Mexico utilized psilocybin-containing mushrooms in their healing rituals to gain insight into illness and promote well-being.
Similarly, the Bwiti religion in West Africa used ibogaine from the iboga plant to facilitate spiritual growth and community.
Scientific Research on Psychedelics and the Nervous System
The renewed interest in psychedelics for healing stems from their rich historical use as promising scientific studies.
Key research includes:
Johns Hopkins University Study:
A randomized, double-blind study led by psychedelic researcher Dr. Roland Griffiths showed that psilocybin could significantly reduce depression and anxiety in cancer patients.
The positive effects were long-lasting, pointing to the potential healing of underlying neural dysregulation.
Imperial College London Research:
Neuroscientist Dr. Robin Carhart-Harris led a study using fMRI scans to investigate the effects of psychedelics on brain connectivity.
The metrics suggested that psychedelics enhance global connectivity, dissolve the ego, and allow different regions to communicate more freely, potentially restoring balance to a dysregulated system.
MAPS-sponsored MDMA Studies:
The Multidisciplinary Association for Psychedelic Studies (MAPS) recently completed its second Phase III clinical trial on MDMA-assisted therapy for PTSD.
Meanwhile, the organization’s first phase III trial showed that 67% of patients no longer had PTSD after three psychedelic therapy sessions. These successful outcomes illustrate how MDMA can effectively heal trauma underlying nervous system dysregulation.

Nervous System Regulation Using Psychedelics
Psychedelics’ potential to regulate the nervous system begins at a neurological level.
Neuroplasticity
Psychedelics appear to enhance neuroplasticity. A fundamental process, neuroplasticity, “is defined as the ability of the nervous system to change its activity in response to intrinsic or extrinsic stimuli by reorganizing its structure, functions, or connections…”
In a well-regulated body, neuroplasticity enables learning, adaptation to new experiences, and recovery from injuries or stress.
In a dysregulated state, the nervous system can become stuck in chronic stress responses, producing excessive stress hormones and creating an imbalance in neurotransmitter activity. This imbalance can inhibit the brain’s ability to form new connections and may even lead to the atrophy of specific neural pathways.
Psychedelics can help unwind that process.
By stimulating 5-HT2A serotonin receptors throughout the central nervous system, psychedelics increase network connectivity and strengthen synaptic communication in areas that might have previously withered.
This process, known as “global functional connectivity,” helps the brain break out of rigid, maladaptive patterns that can lead to mental and physical health issues and forge new pathways that facilitate a dynamic and resilient nervous system.
The Default Mode Network
Psychedelics alter biochemical signaling across the brain’s entire system of networks and regions in extraordinarily complex and non-specific ways. Still, significant mental health research focuses on how psychedelics affect the default mode network (DMN).
The default mode network consists of brain regions including the posterior cingulate cortex, inferior parietal lobes, ventral anterior cingulate cortex, hippocampus, and precuneus regions. These brain regions are most active when the mind is wandering, self-obsessing, and worrying about the future or the past.
Research indicates the DMN is intimately tied to the body’s autonomic nervous system. Therefore, an overactive DMN could disrupt normal functioning, leading to constant rumination and hypervigilance.
Research indicates psychedelics largely decrease activity in the DMN, leading to a “dissolution” of the DMN-fueled ego, replaced by a sense of unity or interconnectedness. This decrease in DMN activity is also a key component in breaking rigid, maladaptive patterns of thinking and behavior, allowing for greater flexibility, quality of life, and adaptability in stressful situations.
Curious about exciting opportunities as a psychedelic practitioner?
Curious about exciting opportunities as a psychedelic
practitioner?
practitioner?
Our FREE E-Book, "Top 3 Emerging Psychedelic Careers," offers a guide to navigating the psychedelic industry.
Plus, you'll receive an exclusive webinar where you can dive deeper and explore these potential career paths.
Psychedelic-Assisted Therapies for Nervous System Dysregulation
Psychedelic-assisted therapies (PAT) have emerged as a novel approach to treating nervous system dysregulation’s underlying causes and effects. This method, involving professionally guided, high-dose psychedelic sessions, offers an integrative strategy for addressing mental, emotional, and physiological imbalances.
Psychedelic-assisted therapy takes many forms, including group ceremonies, plant medicine retreats, and one-on-one sessions with medical professionals like nurses and psychotherapists. Varied approaches allow personalized treatment plans to align with individual needs and goals.
Looking for qualified coaches, therapists, and facilitators who specialize in guiding psychedelic journeys? Visit Third Wave’s Psychedelic Directory to find the support you need to navigate therapeutic experiences safely and meaningfully.
Types of Psychedelic-Assisted Therapies
1:1 psychedelic-assisted therapy:
Individual psychedelic therapy sessions involve a trained medical professional guiding patients through a controlled experience to address mental health challenges.
The process typically begins with preparation sessions where the therapist and patient work together to establish trust, set intentions, and prepare for the psychedelic experience. This stage includes a detailed assessment of the patient’s mental health, medical history, and specific symptoms.
During the psychedelic therapy sessions, which often occur in clinics, the patient ingests carefully measured high doses, and the practitioner remains present, providing support, empathy, and guidance as the person explores their inner landscape.
Group ceremonies:
Group experiences occur in various settings, like psychedelic churches, retreats, and underground circles worldwide. Trained and experienced guides lead these sessions, utilizing collective energy to steer individuals through their therapeutic journey.
Despite the communal atmosphere, participants do not typically interact during shared psychedelic ceremonies. Instead, they often lie on a mat with an eye mask, focusing on the inner experience.
Facilitators typically play music throughout the group experience to facilitate healing while asking participants to remain silent. This process allows people to focus on their subjective visions, sensory perceptions, and lessons.
Psychedelic retreats:
Plant medicine retreats are organized, immersive experiences that offer psychedelic sessions within a supportive container, often incorporating indigenous healing wisdom.
Ayahuasca retreats often occur in a sacred temple under the guidance of a shaman or wisdom keeper with extensive knowledge of plant medicine and spiritual realms.
During the ceremony, the shaman may use various tools like chanting, singing sacred songs called icaros, rhythmic drumming, and other ceremonial practices. These practices help align the energies of the group and allow people to navigate the often intense and profound hallucinatory state.
Benefits and Risks of Psychedelic-Assisted Therapies
Whether in a group setting, sacred temple, or medical clinic, psychedelic-assisted therapies offer diverse pathways toward healing.
Psychedelics allow individuals to access and address underlying issues that conventional therapies might not reach, while enhancing one’s ability to change through neuroplasticity. This powerful combination supports long-lasting therapeutic effects for nervous-system-related conditions like depression, PTSD, anxiety disorders, and addiction.
However, long-lasting doesn’t necessarily mean permanent. Relapsing is a significant risk.
In a recent Andrew Huberman podcast, Dr. Robin Carhart-Harris admitted that, more often than not, people relapse in about three months following the psychedelic therapy experience. From his perspective, and that of most psychedelic experts, post-session integration is critical to mitigating this problem.
Psychedelic integration often involves discussions, reflection, and continued guidance from a therapist, shaman, or experienced facilitator to help people make sense of the journey and reinforce neuroplasticity by applying the insights into real changes in daily life.
“Life is a journey like the [psychedelic] trip is a journey, and there’s always work to do. So the [integration] work is ongoing. But [psychedelics give] people a foot up. It enables people to do the work more easily… That’s very true of classic psychedelics and also very true of MDMA therapy for post-traumatic stress disorder. It’s really making it easier to do very difficult work, going back to a trauma, to digest it, process it, integrate it.” – Dr. Robin Carhart-Harris.
Whether through integration therapy or personal practices like meditation and breathwork, patients must lead the charge in continuing holistic healing practices for the rest of their lives.

Regulate Your Nervous System with Psychedelics: Personal Stories & Case Reports
Fascinating case reports reveal psychedelics’ transformative ability to start people on the path to nervous system regulation.
Annick’s Story
In 1961, a French child psychiatrist described a patient suffering from functional dystonia, a movement disorder affecting her lower extremities. At age 13, Annick began complaining of left foot pain and displayed challenges walking.
She continued limping through age 16 when a minor trauma led to pain in her other foot. Despite reporting a normal family life, Annick often awoke in fear that a man resembling her father was in her bedroom. In addition to pain, Annick displayed enduring “hysterical” behavior and anxiety.
After three weeks in the hospital, Annick’s doctor injected her with 9 mg of psilocybin. The result was nothing short of miraculous.
At the end of 2 hours, she declares that she must absolutely say certain things that she has never said before …. She confesses then that her father and mother are inveterate alcoholics … and that the arguments and the violence of which they are both guilty create an unbearable family life.
Indeed, the apparent inner liberation which accompanies these declarations is of greater interest than their very content. Nonetheless, in six years, this is the first time she gives details about her parents, a subject she had always avoided previously; even during the narco‐analyses, this problem had never been addressed.
In the following days, we very quickly witness the disappearance of the troubles and the resumption of a perfectly normal gait.
Lori’s Story
For Lori Tipton, a MAPS MDMA clinical trial participant, PTSD came in the form of Hurricane Katrina, her brother’s overdose, her mother’s murder-suicide, and a rape that occurred years later.
In a quest to heal, Lori took antidepressants, anti-anxiety pills, and ADHD medicine. Nothing got to the core of the problem. Medications masked the symptoms while eliminating her motivation to live life fully.
Featured in Michael Pollan’s How to Change Your Mind docuseries, Tipton recalled how MDMA therapy changed everything.
One of the beautiful things that came out of [MDMA therapy] is that I was able to finally be present to my life. Because of my PTSD, it robbed me of my own life for years… So to be in an experience wholly, not just your mind, not just your body. But to be wholly present for something is such a gift. Because that’s where we have the capacity for the most joy, or the most pain, or whatever it is. But at least we feel it, and we know it’s real, and we experience it, as opposed to living dully in a life where you’re constantly afraid, where you can’t access the love that surrounds you.
The Bottom Line
Psychedelics’ potential to heal a dysregulated nervous system is a fascinating exploration of the mind, body, and soul. Merging the wisdom of ancient rituals with cutting-edge neuroscience, psychedelics open doors to profound emotional insights and new neural pathways of healing.
They offer a compassionate embrace to those seeking solace from physical and mental health challenges, connecting them to a world of empathy, understanding, and transformation. Psychedelics paint a picture of hope and nervous-system renewal.
Ready to re-balance your internal landscape and accelerate your professional career? Third Wave’s Personalized Psychedelic Coaching program includes one-on-one coaching calls, psychedelic skills training, a virtual breathwork ceremony, and lifetime access to its community for invaluable support.








Thank you! Are there considerations for using these substances for entities such as Parkinson’s
Harry Presberg, M.D.