Collaborative Care: Building a Psychedelic-Assisted Mental Health System
LISTEN ON:
Episode 209
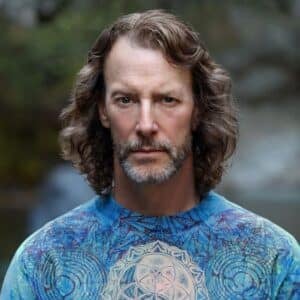
Jonathan Sabbagh
In this Psychedelic Podcast episode, Paul F. Austin welcomes Jonathan Sabbagh, CEO of Journey Clinical, who shares his mission to integrate FDA-approved psychedelics within the modern therapeutic framework.
Jonathan highlights the disjointed nature of today’s mental health system, where therapists and prescribers lack communication, hindering comprehensive assessments and referrals. He and Paul emphasize Journey Clinical’s collaborative care model, streamlining information exchange, and maximizing psychedelic-therapy access through telemedicine innovation. They explore Journey’s potential challenges of scalability, therapist training, and insurance coverage for extended sessions. And they consider the balance between state-level decriminalization, psychedelic medicalization, and decentralized access.
Join Paul and Jonathan as they imagine a new mental healthcare infrastructure that addresses the growing crisis and reinvents therapeutic care as we know it.
Jonathan Sabbagh:
Jonathan Sabbagh is the Co-Founder and CEO of Journey Clinical, the leading telehealth platform expanding access to psychedelic-assisted psychotherapy. A serial entrepreneur, Jonathan built his career in finance, spending over two decades working for hedge funds and building businesses in Switzerland and NYC.
After receiving a difficult diagnosis of PTSD and extreme burnout, Jonathan left the world of finance to focus on his mental health. During that time, he personally experienced the transformative benefits of plant medicine and ketamine-assisted psychotherapy (KAP). Jonathan’s healing journey inspired him to begin formal clinical psychology training at the New School, with the vision of expanding access to transformative psychedelic-assisted therapies to the millions of Americans with depression and anxiety.
Jonathan’s personal and professional journey motivated him to found Journey Clinical in 2020, the #1 platform in the US that enables licensed mental health professionals to deliver KAP at scale.
Podcast Highlights
- How Jonathan’s mental health & finance background led him to start Journey Clinical.
- Jonathan’s take on co-founding and running Journey Clinical with his wife.
- The origin story of Journey Clinical and its startup challenges.
- Exploring Journey’s collaborative care model.
- Investigating Journey’s infrastructure solution for psychedelic-assisted therapy.
- Journey’s vetting requirements for network therapists.
- How the Ryan Haight Act might affect ketamine telehealth access.
- Journey’s decentralized approach to safe and responsible ketamine telemedicine.
- Integrating FDA-approved psychedelics into the mainstream mental health infrastructure.
- Jonathan’s long-term vision for collaborative mental health care through Journey Clinical.
Show Links
- Journey Clinical
- Journey Clinical on Instagram
- Jonathan on Instagram
- Jonathan on Twitter
- Union Square Ventures
- Ryan Haight Online Pharmacy Consumer Protection Act of 2008
- MUDWTR founder Shane Heath’s article in Business Insider on startup hustle culture
- Spravato prescription ketamine
- (clinical trial) At-home, sublingual ketamine telehealth safety study
- The Ultimate Guide to Ketamine
- (blog) Ketamine Treatments at Home: Find Wellness While Wearing Your Fuzzy Socks
- (blog) Why Ketamine Could Replace Antidepressants
- (blog) Why Aren’t More Doctors Talking About Ketamine Therapy?
This episode is brought to you by Psyched Wellness. Their product, Calm, is an over-the-counter Amanita muscaria extract that may help to reduce stress, ease muscular tension and promote restorative sleep. Their team of leading scientists and wellness professionals has managed to successfully distill the restorative and healing elements from the Amanita muscaria mushroom.
To be one of the first to try this breakthrough product, go to shop.psyched-wellness.com and use the code THIRDWAVEPOD to get 15% off when ordering.
This episode is brought to you by Apollo Neuro, the first scientifically validated wearable that actively improves your body’s resilience to stress. Apollo engages with your sense of touch to deliver soothing vibrations that signal safety to the brain. Clinically proven to improve heart rate variability, it can actually enhance the outcomes of your other efforts like deep breathing, yoga, meditation, and plant medicine. Apollo was developed by a friend of Third Wave, Dr. David Rabin M.D Ph.D., a neuroscientist and board-certified psychiatrist who has been studying the impact of chronic stress in humans for nearly 15 years. Third Wave listeners get 15% off—just use this link.
Podcast Transcript
0:00:00.5 Paul F. Austin: Hey listeners, welcome back to The Psychedelic podcast. Today we have Jonathan Sabbagh, the co-founder and CEO of Journey Clinical.
0:00:08.9 Jonathan Sabbagh: To me, the number one healthcare crisis in the world today, it's not cancer, it's not obesity, it's mental health. And so we're having to find ways to essentially innovate in an area that really hasn't seen much innovation in the past 50 years, especially mental health. And so psychedelics are the first paradigm shift that emerges, I think bringing in the collaborative care model, working with therapists, being an infrastructure solution to us seem the most scalable and sustainable way to do it.
0:00:44.9 Paul F. Austin: Welcome to the Psychedelic podcast by Third Wave, audio mycelium, connecting you to the luminaries and thought leaders of the psychedelic renaissance. We bring you illuminating conversations with scientists, therapists, entrepreneurs, coaches, doctors and shamanic practitioners, exploring how we can best use psychedelic medicine to accelerate personal healing, peak performance and collective transformation.
0:01:17.1 Advertisement: Today's episode of The Psychedelic Podcast is brought to you by Psyched Wellness. Psyched Wellness has this amazing product, it's called CALM, and it has been developed by wellness professionals, along with leading scientists, and is the very first over-the-counter Amanita muscaria extract that may help you reduce stress, ease muscular tension, and promote deeper more restorative sleep.
This natural supplement is lab-tested, it's been detoxified and it is fully safe for consumption. For the first time in modern history, scientists working with Psyched Wellness have successfully distilled the restorative and healing elements from the Amanita muscaria mushroom and placed them into a powerful extract that is now the first legal Amanita muscaria extract available for sale in the USA. If you would like to be one of the first to try this breakthrough product, then you can go to shop.psyched-wellness.com. That's shop.psyched-wellness.com, and use code, THIRDWAVEPOD that's Third Wave pod, P-O-D, to get 15% off when ordering. Again, that is shop.psyched-wellness.com and use code, THIRDWAVEPOD to get 15% off your order.
0:02:45.7 Paul F. Austin: Hey, listeners. Welcome back to the show today, Jonathan Sabbagh, the co-founder and CEO of Journey Clinical is joining us. Journey Clinical is the leading telehealth platform, expanding access to psychedelic-assisted psychotherapy. And Jonathan, as a serial entrepreneur, built his career in finance spending over two decades working for hedge funds and building businesses in Switzerland and New York City. After receiving a diagnosis of PTSD and extreme burnout, Jonathan left the world of finance to focus on his mental health. During which time he personally experienced the transformative benefits of ayahuasca and ketamine-assisted psychotherapy. Jonathan's personal healing journey inspired him to begin formal clinical psychology training at the New School with the vision of expanding access to transformative psychedelic-assisted therapies for millions of Americans living with depression and anxiety. And I meant to interview Jonathan for the podcast for over a year and a half. Now, we finally had the opportunity to sit down and hear about Journey Clinical's model to democratize access to psychedelic-assisted psychotherapy.
0:03:50.1 Paul F. Austin: We talked about the importance of collaborative care, we went deep into how ketamine is a wedge, but what about psilocybin and LSD is the real psychedelics. And then we also got into the Ryan Haight Act, which is a legislative bill that will impact the ability for ketamine-assisted psychotherapy to be delivered from a telehealth perspective and lens. This was another excellent conversation with an entrepreneur of integrity, building something of value in the space. And so it really is an honor to bring this to you here today. So without further ado, I bring you Jonathan Sabbagh, the co-founder and CEO of Journey Clinical.
0:04:36.3 Paul F. Austin: Hey listeners, welcome back to The Psychedelic podcast. Today we have Jonathan Sabbagh, the co-founder and CEO of Journey Clinical, a mental health startup that is building an infrastructure to empower independent psychotherapists to democratize access to psychedelic treatments, starting with ketamine. Now, Jonathan, we had an opportunity to meet a year and a half ago, at Wonderland in Miami, you have made incredible strides since that point in time, and so it's fun to be able to sit down with you now and chat a little bit.
0:05:06.7 Jonathan Sabbagh: I'm glad to be here, thanks for having me.
0:05:09.5 Paul F. Austin: So you are one of the few, I would say, non-biotech psychedelic companies that is supported by, I would consider the gold standard, one of the gold standards of venture fund, Union Square Ventures. And I'd love to talk in depth today about Journey Clinical, about the model that you're building, about why you think it's the future, about how it democratize access, all those sorts of things. And let's first start with your journey and your story. You're now living in New York City, you've raised a significant amount of funding for Journey Clinical as an entrepreneur, is this your first entrepreneurial project? Why is it that you chose psychedelics and mental health as a focus? And maybe just tell us a little bit about your own journey as a human, and how you've helped... How you've healed and really transformed through therapy, through potentially intentional psychedelic use, all those sorts of things.
0:06:13.8 Jonathan Sabbagh: Yeah, sure that's a great question. So my background, I grew up in Switzerland, and for the most part of my professional life, I worked in finance. I spent pretty much 20 years working in that field, mostly in hedge funds. I built two businesses from the ground up. We were working in illiquid assets back then. And when I was building that very first company, I actually experienced a very substantial burnout, which turned out to be the result of undiagnosed post-traumatic stress disorder. But I didn't know that, and so I spent most of my adult life dealing with depression, anxiety and substance abuse. And until about eight years ago, I really found myself on a downward spiral. And a friend of mine recommended that I try ayahuasca. And so he brought me to a traditional Ayahuasca ceremony here in New York. And it was a really very substantial experience for me, and I actually did seven in this course of two weeks right after that, and many more since. And I spent two years working with that medicine. It was... It's corny to say this, but it really saved my life, it really changed my life, it was a very determining moment in my personal journey.
0:07:31.5 Jonathan Sabbagh: It was the first time that I had the chance to observe the inner conflict that I was feeling and understand how much pain I was going through actually. And after a while, what happened was that I really couldn't process those ceremonies anymore, it was kind of in a loop, and I would, kept having the same ceremony over and over again, and the experience kept getting harder and harder. And so at some point I decided to seek help, and so I reached out to find the therapist in New York that was able to help me understand and integrate these experiences. And so I found someone really awesome, and we started working with ketamine-assisted psychotherapy. And for the first time in my life, at the age of, I think it was 37 or something, I was diagnosed with post-traumatic stress disorder, which was... Oddly enough, a pretty big relief because living with something that you don't quite understand and that you feel it's trying to harm you when in fact, it's all about accepting yourself was very relieving for me.
0:08:36.7 Jonathan Sabbagh: And so we did a lot of work for almost two years with ketamine-assisted psychotherapy. And in the course of that journey for myself, I led a more integrative life, I felt much better, but I also started to feel a bit of a disconnect with the career that I had chosen and I just couldn't find a sense of purpose in it. And so I really took a break for a while, and I landed on the fact that I really loved psychotherapy. I loved being in therapy, but I was also very passionate about the field of psychotherapy. And so I decided to quit finance and go back to school at the age of 38 to study clinical psychology here in New York. And I actually... I had to pass my GED 'cause I hadn't finished high school when I went into finance. So I had to go and do my GED here in New York. It was a really inspiring experience because I found myself in Far Rockaway with other people who were 40, who were doing their GED, and I was so impressed by all of these people taking their life in hand and moving it forward. And so that was really awesome.
0:09:42.9 Jonathan Sabbagh: And then I went back to school as an undergrad to study clinical psychology at the New School here. And while I was doing that process, I got accepted in the master's program, and I felt the need to integrate all of that background that I had as an entrepreneur, with my long-term goal of enabling better access to these treatments at scale. And I think this is a common theme with people who walk this path, is that you don't... You change, but you don't change, right? You are who you are, and I think what you change is your perspective on who you are. And so that was really empowering to me, and so I felt that... I did all this work and I am an entrepreneur, I enjoy being an entrepreneur. I also am passionate about therapy and psychedelics, and so this was very natural. And so that's when I decided to found Journey, and I also had the chance and the pleasure of having my wife become my co-founder and so that's how we got started.
0:10:41.5 Paul F. Austin: Let's go there. What is it like to have your wife as a co-founder?
0:10:46.2 Jonathan Sabbagh: It's pretty amazing. It's pretty intense.
0:10:49.4 Paul F. Austin: Yeah.
0:10:49.8 Jonathan Sabbagh: The first... I think we hated each other for the first six months of building the company when we really got started. You know, you build a relationship with somebody who you really know as your partner and your partner in life, but then you discovered this whole other personality that you then have to make friends with and learn how to exist with and evolve with. And so that was the beginning of our journey. But then we did a lot of work on ourselves. We had coach... We have coaches, therapists. And I find that it's my favorite thing, actually, I wouldn't wanna do it with anybody else because we have a joint vision, our interest are aligned, we care about the same things, and so I absolutely love working with my wife. She's also... She happens to be an absolutely awesome operator. So that's a huge deal, but as a human, I have the pleasure and the privilege of spending all of my time with my best friend, with my wife and with the best co-founder I could have found.
0:12:01.7 Paul F. Austin: That's fantastic, 'cause that's one of those things that could go amazing and could also go incredibly sideways, and one of the biggest reasons companies fail, I would say the biggest reasoning companies fail, startups fail is because of co-founder conflict. So knowing that you had, I'm sure like a stable healthy relationship prior to starting Journey Clinical, it's probably even a good signal to investors or a good signal to your community that birthing this new thing, this new company between you two is something that has a lot of upside because you don't have to... You know her intimately. You don't necessarily need to worry about, am I gonna gel with this person or not? Well, I've seen this time and time again in the psychedelic space and many other industries that you meet someone, six months later, you've started a business with them, and then another six months later you're wondering why they are the way that they are, right?
0:13:09.1 Jonathan Sabbagh: Correct.
0:13:09.6 Paul F. Austin: So to have that opportunity to already know some of those shadows, and of course, it's a whole another... You're working at a whole another level when you have all these elements coming together, and yet you've been very successful so far with Journey Clinical. Just tell us a little bit about the journey so far from a purely business lens, and then we'll get more into the healing and psychotherapy side. But just from a business lens, the psychedelic space is hot, there's been, I think, over $2 billion dollars of investment that has come in to the space. The vast majority of that is in drug development and biotech, which you are not doing. What are some of the things that have inspired you? What have been some of the challenges just in the early stages of starting to build and grow Journey Clinical.
0:13:55.4 Jonathan Sabbagh: Yeah, I mean, we're building a health tech startup, right? That's what we are, that's what we're building. We're building an infrastructure solution, and so every challenge that applies to every early stage tech or health tech startup applies to us. And I think that's a really important thing to distinguish, sometimes people have this idea that because we're in the psychedelic space, challenges are different or perspectives are different or dynamics are different, and they're not. We are operating essentially in a certain system, and so every challenge that every founder faces building a large company at an early stage can apply to us. And so it was fundraising and then proof of concept showing that you can achieve growth, hiring, more fundraising, retention, revenue optimization. I mean, everything that everybody else deals with, we deal with as well. So I think that's been for us, our experience. I think that we have the privilege to be stewards to a model that enables healing and that has a virtuous circle built into it. But we are a venture-backed start-up, and so we have to be conscious of those dynamics and abide by them.
0:15:21.4 Paul F. Austin: Fundraising, I put product market fit, growth, hiring, retention, you mentioned that you exist within the system of being a health tech start-up in particular, what... Not even looking out at the psychedelic space, but to just broadly zooming out about health tech, what are some of the challenges or some of the problems that we're looking at from a health tech perspective that you think Journey Clinical can really help to address?
0:15:43.5 Jonathan Sabbagh: Yeah, that's a great question. We exist in a western medicine model, and we exist in a western model, or western capitalistic model where insurance payer, access to treatments, quality of care at scale, accessibility to these treatments are the issues that we're facing. I think that to me, the number one healthcare crisis in the world today, it's not cancer, it's not obesity, it's mental health. And so we're having to find ways to essentially innovate in an area that really hasn't seen much innovation in the past 50 years, especially mental health. And so psychedelics are the first paradigm shift that emerges, and so now the challenge is to bring them sustainably at scale. I think bringing in the collaborative care model, working with therapists, being an infrastructure solution to us seemed the most scalable and sustainable way to do it. And so I think that's the challenge. The next challenge will be how to get insurance to cover this and increasing quality of care at scale, like building large systems are complicated. And building a large medical system is very complicated and expensive. So I think these are... I think, the main challenges that we're seeing and we're gonna wanna enable accessibility in all areas, not just large cities, so that's why we landed on this model.
0:17:11.4 Paul F. Austin: You mentioned this a couple of times, the collaborative care model. Can you expand on that? What is a collaborative care model?
0:17:17.6 Jonathan Sabbagh: Of course. So a journey, for example, what we do is we partner with licensed mental health professionals to enable them to deliver these treatments in their practice as an adjunct to therapy. There are other models or other companies that work with a collaborative care model. And the idea here is that the medical team partners and collaborates with the therapist to deliver essentially what is a bespoke treatment plan at scale. And so it's very odd, if you think about it, that today, someone is seeing a therapist once a week, and this person has a tremendous amount of insight into their mental health, into their progress, and there is zero communication in most times between the therapist and the prescribers of these treatments, right? This is completely disjointed. And that makes no sense, like how can the prescriber assess how the medical treatment that they're prescribing to this patient is impacting their mental health, they're not communicating with a therapist who's actually working on processing all those insights and that patient's mental health on a regular basis. And so that's the collaborative care model. It's bringing in the therapist with the medical team and building essentially what is concierge mental health at scale.
0:18:34.0 Paul F. Austin: And you're doing that with ketamine-assisted psychotherapy, and I'd love if you could just talk a little bit about how that's going so far. What are you optimistic about as it relates to the sort of decentralized model, this collaborative care model for ketamine, and what are some of the challenges or risks that have started to present, including maybe talk... I would love... This might be a good opportunity to talk a little bit about the Ryan Haight Act and sort of what's happening there from a legislative perspective.
0:19:07.9 Jonathan Sabbagh: For sure. I think maybe it might be helpful to start about explaining what we do a little bit.
0:19:12.2 Paul F. Austin: Let's do that.
0:19:14.0 Jonathan Sabbagh: We've built and then I can, I'm happy to digress into the Ryan Haight changes. So as I said, what we identified is that enabling these therapists to incorporate these treatments in their practice as an adjunct to therapy is what we believe is going to increase accessibility sustainably. And so today there's about 40 million people in therapy in America, so it's a huge population. And what we tried to look at was what was the main barrier to entry for these therapists who have a therapeutic alliance with their patients to enable them to include these treatments in their practice. And what we found after interviewing 600 of them was that forming and maintaining relationships with prescribing physicians is actually the hardest part. There's only 25,000 psychiatrists in America today, and they're mostly located in large cities. And there's an equal shortage of psychiatric nurse practitioners, and for the most part, none of them are psychedelically-informed. And so when they have these relationships, they're often fickle and they put a lot of pressure on the cost for the patient and the therapist, which doesn't enable them to increase their revenue.
0:20:20.5 Jonathan Sabbagh: And so what they do for the most part is refer out, they'll refer out to clinics or direct-to-consumer platforms. And if you're a patient, if you're in therapy, it probably took you a lot of time to find a therapist that you like and to build a therapeutic alliance. And now you're being asked to have what is potentially the most cathartic experience of your life with someone you've never met or an app. And that's just not great from a patient's perspective. And so it's important to understand what we're building at Journey Clinical. We're not a ketamine company, we're not a direct-to-consumer offering, we're an infrastructure solution. We're essentially the missing link for psychedelic-assisted psychotherapy to exist. Without it, the network of therapists cannot incorporate this treatment in their practice. And so what that means is that we set them up with everything they need to incorporate for now, ketamine-assisted psychotherapy, starting with a Telehealth platform, where our in-house medical team takes on all of the medical side and our member psychotherapist takes on all of the therapy. So practically, how this works is that, as I said, we support a collaborative care model, so these therapists will refer their patients to Journey Clinical, our team will see them for a full-hour intake, if they're eligible for the treatment, we'll send them sublingual ketamine to their home enough for two sessions.
0:21:40.0 Jonathan Sabbagh: Those two sessions are delivered by their therapist, and we support a variety of protocols. There is an at-home protocol, in-person, remote, group protocol, remote group, we have a retreat protocol, we even have couples protocol. And the reason why we have so many protocols is because the therapist needs to have flexibility in their practice to deliver these treatments as best matches their practice, but also the patient needs to have flexibility. Some patients wanna start in-person and might wanna do at-home after. And so giving flexibility is really, really important. Then once they had those treatments, they come back for dose adjustments and we see them regularly for follow-up consultations. The other part, and I think this is really what we do at Journey, it's not prescribing ketamine, it's this collaborative care model. Because when... And for example, a difficult experience occurs, these therapists have 24/7 access to a world-class medical team, and we're there to support them and the patient when these events occur. And so that triangulation really mitigates negative outcomes. But the other side of that is that we collaborate regularly to build a bespoke treatment plan for the patient, because we don't believe that there is a cookie-cutter approach to this. We don't believe that people do six sessions a month and just keep doing it.
0:23:00.2 Jonathan Sabbagh: People, everybody has different needs. There are no medications in the world that has a standardized treatment model. And so specifically this one, some people needed a lot of it in the beginning, they don't need it for a while, maybe an event happens and they need it again. And so the ability to work with a therapist and the patient to deliver the right treatment plan is what we offer here. And then all of this is tech-enabled, we have EMR for our prescribers, we have a whole platform for the therapist, there is training. Fluence designed a 22 module training for us. We have experiential learning, we have peer consultation groups, therapists can experience a CAP session led by other Journey members. We have a lot of peer-to-peer dynamics, we have a lot of community offerings, they have access to our medical team regularly. We put a lot of content out, like this webinars on consent to touch and scope of practice and IFS and CAP, and we do a lot of things. We give them marketing resources, we give them legal resources like informed consent forms, and then it's all HIPAA compliant so it's very easy for them to refer their patients through their portal. They log their sessions through that, and they can track outcomes and communicate with the prescribers through there, and then there's a patient portal.
0:24:07.5 Jonathan Sabbagh: And so today we have... We opened our membership in end of February of last year, we had 30 members, and we have about 800 therapists in our network today in multiple states. We've seen about 2,000 patients during that time, and I just saw that through our network, our therapist delivered 3,500 CAP sessions during that period. So it's really cool to see that over the time. And we even saw that, I think it's about 92% of our patients reported improved outcomes. So it's been really an interesting journey of growing fast and growing well.
0:24:45.6 Advertisement: Hey, everybody. I hope you are enjoying today's episode of The Psychedelic Podcast, which has been brought to you by our good friends and makers of the Apollo. The Apollo is a wearable that, well, you can put just about anywhere; on your wrist, on your ankle, on even on your shirt collar, and it will improve your body's resilience to stress, improve your focus, and even deepen your sleep. Developed by neuroscientists and physicians, the Apollo delivers gentle, soothing vibrations that recondition and recalibrate your nervous system over time. It's like a remote control for how we want to feel throughout the day; more energetic, less stressed, happier mood, calm and relaxed and sleepy at night, which is why Third Wave's founder, Paul Austin, has referred to the Apollo as "a microdose on your wrist." The Apollo wearable is the only technology with an issued patent to reduce unpleasant and undesired experiences associated with both psychedelic and traditional medicine-assisted therapies.
In studies, users of the Apollo have experienced up to 40% less stress, less feelings of anxiety, 19% more time spent in deep sleep, and up to 25% increases in focus and concentration. The Apollo wearable, unlike a whole new morning routine or a new meditation practice, although those things are great, is a simpler thing to do each day. You put it on your body like a wristwatch and vibe your way to very real world results and a whole new level of stress resilience in your daily life. And right now, Psychedelic Podcast listeners can save $50 on the Apollo wearable by visiting apolloneuro.com/thirdwave. That's apolloneuro.com/thirdwave. Now, back to the show.
0:26:39.3 Paul F. Austin: So, just to step back a sec... I fully understand this and it will probably help to clarify for the audience as well, so the therapeutic alliance is established, a therapist is working with a client, and then maybe like three months after that, six months after that, a year after that, that client is still struggling with X, Y and Z issue, and the therapist has maybe heard about ketamine-assisted psychotherapy, and you make it really easy for them to sign up, to pay a monthly membership fee, which gets them access to this entire backend. I mean, the therapist himself can't prescribe the ketamine, but you have the medical team that can prescribe the ketamine and the therapists can work with that individual with the ketamine-assisted psychotherapy approach.
0:27:20.0 Jonathan Sabbagh: Exactly.
0:27:20.6 Paul F. Austin: Is simply... Am I understanding that correctly?
0:27:21.2 Jonathan Sabbagh: That's correct. Yeah, 100%.
0:27:22.7 Paul F. Austin: And, so that's the case. Do you have any situations or whether it's the percentage or whatnot of simply therapists who are already trained and certified and psychedelic-assisted psychotherapy, maybe they... And they're looking to specifically get clients who wanna work with ketamine, is that a common or popular thing, or is it usually focused on therapists who already have a ton of clients, they already have a therapeutic alliance and now they're just weaving in ketamine. It's more the former, maybe that... I don't even know if that question make sense now that I'm at 59.
0:28:06.2 Jonathan Sabbagh: No, I understand what you're saying. So we've got a broad spectrum of different profiles that are in our network. So some therapists are highly trained, they've done CAP training and MAPS training and they're super experienced, and they basically wanna plug in to essentially that backend infrastructure where we're basically becoming their in-house doctor, right? So they have... It's very easy, it's very affordable... It's also very affordable for the patient, like we only charge 250 for an intake and 150 for a follow-up. We're able to do that in part because we do charge a membership fee, so it's a virtuous cycle where if they do well, we do well. So we've got people who are super experienced, we have people who have never ever done any kind of training, who are interested in adding this and who start from scratch, and our whole infrastructure allows them to do it within Journey. They don't have to go out else where. They even get CE credits for the training. So that's all embedded in there. And then we have people in the middle who have some patients who said, "Look, I'm really interested in this, I'd like to try it out, and can you do this for me?" And then we have newer therapists who require patient referrals, so we're building that out as well. But for the most part, our patients are referred to by the therapist.
0:29:18.2 Paul F. Austin: Do you have any like... Or I should say, what are your vetting requirements for therapists who are looking to register and sign up. I mean, you don't require them to have, for example, the MAPS or the CIS, because you have something built with Fluence that they can get the CE. Do you require them to have been in practice for a certain number of years or to be in certain cities, or is it as long as they have a license and they have clients that they are able to sign up for what Journey Clinical is offering?
0:29:52.4 Jonathan Sabbagh: Yeah, so we only work with licensed mental health professionals, and so becoming licensed is actually a lot of work. They have to go to school, they to have internships and they have to have a certain amount of hours to be licensed, and so that's a pretty high barrier to entry in itself. In terms of the trainings, if they've taken another training, they don't have to take our training. That's fine. If they haven't, they have to take our educational videos and go through all the process. So that's one part. And another thing that I didn't mention is that there's a huge amount of community offerings, and I think that's something that people don't realize is how lonely it is for a therapist to be a therapist, it's a lonely job. And so having access to a community of peers, or the peer consultation groups to meet ups to having an accountability partner. So there's a whole infrastructure in place that really allows them to connect, which is why we've really successfully had people who'd never tried this, never worked with these compounds in their life and started their journey from scratch and build pretty amazing practices.
0:30:53.6 Paul F. Austin: Incredible. Okay, let's get into the Ryan Haight Act now, 'cause it's something that is currently being discussed by the DEA, the sort of brief context for our listeners that I'd love for you to dive in deeper about what's currently happening is when Covid hit, there was a loosening of regulations around telehealth prescriptions. And now with the Covid emergency being officially over, there's conversation about shifting that back to not exactly what was present pre-Covid, but to somewhat of a hybrid model from what I've seen at this point in time. So I'd love if you could just explain to our listeners a little bit about the Ryan Haight Act and how you're thinking about it, how it's potentially impacting Journey Clinic, and what your thoughts and perspectives are around the Act itself.
0:31:54.6 Jonathan Sabbagh: Yeah, for sure. So I think maybe a little bit of context on why the Ryan Haight Act existed in the first place. So about 14 years ago, a young man called The Ryan Haight was prescribed opioids by a compounding pharmacy and overdosed. And so the Ryan Haight Act was put in place essentially to dismantle like pill mills who were prescribing controlled substances without a doctor in place. And when... At the same time, there was a mandate for the DEA to have a telehealth license, which really never was implemented by them. And so as you said, during Covid, those restrictions were lifted. This in-person requirement, which is essentially a vitals check, and then you have to do it every two years was lifted.
0:32:41.5 Jonathan Sabbagh: And so in that time, as we all know, the world kind of evolved and a tremendous amount of telehealth organizations came out and developed, and so there's a lot of positive to what happened because that completely democratized access to these treatments, it reduced cost, it helped people in rural areas get easier access to the treatment that they needed. Things like opioid, Suboxone and opioid addiction treatment were really made very accessible. And the initial fear was that there was gonna be a huge amount of abuse, but it didn't happen.
0:33:15.6 Jonathan Sabbagh: In fact, it made it accessible, the medical consultations online are perfectly fine and perfectly well run. And so then the Biden administration basically kept pushing back the dates of the ending of the PHE and within the PHE was the exemption for this in-person requirement through the Ryan Haight rule. And so I think about a month ago, the DEA issued essentially proposed guidelines, which in essence, require not an in-person evaluation for the prescription of these treatments, but actually it's a referral. So a referral from any practitioner who has a DEA license, and so a referral could be... It could be really from anybody who has a DEA license. So if you're a primary care practitioner or you're a cardiologist or whomever feels like, Oh, I'm gonna refer you to these professionals, and they've seen you in person, there's some quite simple forms that need to be filled in, then that will serve as that in-person requirement.
0:34:19.5 Jonathan Sabbagh: So it's not a very big requirement. There's also an opportunity for a telehealth companies to prescribe, at least at this point in time, the 30 days worth of treatment before that referral happens. There's also a 180-day grace period that's proposed for people who are currently in treatment. So there's a spectrum of flexibility, and all of this is open for commentary. And so to date, I think there's been like 1,800 comments submitted to the DEA on their proposed guidelines, overwhelmingly, really in favor of telehealth and loosening these guidelines. So we'll see exactly what's going to happen. So the commentary period closed and we're now waiting for final guidance from the DEA. So that's where we're at right now.
0:35:07.5 Jonathan Sabbagh: For us as a company, this really doesn't really impact. We're very confident that people will be able to fulfill those requirements through people's existing providers or ones that we can put together. And so that plays into our collaborative care model very well. So for us, we're not particularly worried about this. We have planned for this from the day we launched our company. So we were ready for this, we were never under the idea that we wouldn't have to deal with the change in regulation, and so we had multiple plans that were extremely viable and scalable, that we had put in place. And so, which is also why our investors were confident in our ability to execute. And so we're absolutely ready for this, and we don't anticipate this being any kind of disruption to our business.
0:35:56.6 Paul F. Austin: Yeah, it's interesting because one of the hot topics of conversation has been around ketamine in the psychedelic space, but it has been around how ketamine is not like the "classic psychedelics" and that it does have more potential for addiction. And that some of these telehealth measures are being abused with ketamine in addition to other medications, like I think a big one was like ADHD medications or something like that as well. And, yeah, Mindbloom, who has been a collaborator and I think they've done over 100,000 ketamine-assisted psychotherapy sessions, carried out some research on the efficacy of telehealth ketamine, and it's looking to be basically just as helpful and effective as having to go into a clinic for IV or I'm. So I feel like telehealth is the future, decentralization is the future, and what I'm hearing from you is, no matter which way it goes, and I don't think it'll ever be black or white, there's gonna be shades of gray in terms of that, that Journey Clinical is well set up and equipped to handle that specific to ketamine. Which then leads me to my next question, 'cause this I feel like is the million dollar question from a visionary perspective. Yeah, go ahead.
0:37:17.0 Jonathan Sabbagh: Actually, even before you add that next question, one thing I'll say is that our model is actually a really poor model to abuse drugs, because we require patients to be in a therapeutic alliance with one of our members. It's very onerous for anybody to try to abuse drugs for our platform, and so we're pretty confident that our model is extremely responsible, yet scalable at the same time.
0:37:41.0 Paul F. Austin: And it's important because there are a few ketamine, and Mindbloom is not one of these, but there are a few ketamine platforms where you can simply sign up, you can pay, I believe, a membership fee or a monthly membership fee, and they'll just ship you ketamine, if you want it. They don't necessarily pair you with a coach or a practitioner or a clinician. They're just sending it to your home, which is a little too libertarian, I feel like, for how early we are in this sort of psychedelic renaissance.
0:38:12.0 Jonathan Sabbagh: Yeah, I think it's our responsibility to do this well and responsibly. There are, as you say, like any drug, there is potential for abuse, people can abuse SSRIs, they can abuse a lot of things, and ketamine is very safe as a profile, but we have to do it responsibly. And that's why we built a model where they have to be a therapeutic alliance, we only send them enough for two sessions when they start, they come back, we have to re-evaluate every time if they're eligible for the... There's eligible, if it makes sense, we work with the therapist. So it's a different structure that we've put in place, and that's why also we felt that having the therapist as our primary customer was a very good way to approach this.
0:38:53.6 Paul F. Austin: Let's talk about MDMA and Psilocybin. Now, so MDMA is looking to be approved, they think in 2024 for PTSD. I know MAPS is having to do a lot of work right now to raise additional funds for the commercialization efforts, et cetera, et cetera. Psilocybin, TBD right? Some folks think 2024 or something, folks think 2025. Regulations are a bit up in the air right now in terms of those precise timeline. So let's assume now, at some point, within the next few years, psilocybin and MDMA become FDA approved and medically available for clinicians and psychiatrists to work with. Does your model have to change at all? And the reason I ask for that, or how does your model change if your model changes? And the reason I ask that is because ketamine is a 90-minute experience. Obviously, psilocybin and MDMA are closer to four to six hours. So I'm just curious about your vision in terms of encompassing these other psychedelic medicines that have a much different subjective effect than ketamine.
0:40:10.1 Jonathan Sabbagh: That's a great question. So again, we're a drug-agnostic model. What we're building is infrastructure, we're not focused on one drug. So no one knows yet what the most popular or not maybe not popular, but most effective drugs are gonna be, and so there's hundreds of these drugs in drug development right now, and there's millions of dollars or hundreds of million of dollars going to fund these drug development. So we'll see what kind of new compounds come out in the coming years. For MDMA and psilocybin who are of course the next ones up. It's true, like eight hour sessions is super onerous for a therapist, it's onerous for the patient. I'm curious to see how the insurance companies are gonna be covering that and how open they are gonna be to approving these treatments. So it's like when you get a CAT scan or an MRI and you need to get a pre-authorization. Well, I'm curious to see how that's gonna work. I heard that they're developing codes, however, for MDMA, so that's pretty awesome. So we're gonna see. I think it's all gonna depend on the REMS that come out of the risk and mitigation strategies that are proposed by the FDA, and how much they're gonna require, is it gonna be two therapists, is it gonna be training, is it gonna be...
0:41:24.9 Jonathan Sabbagh: So we'll see. I'm sure all these drug dev companies are gonna push for the maximum flexibility on these REMS because from that depends how successful they are in commercialization. If it becomes a very expensive treatment that only few can afford, then that's gonna be difficult. You also wanna have therapists that are gonna be willing to commit to spending eight hours at a time with their patients, and if you have to have two, that becomes more complicated. So we'll see. For us, it really doesn't quite matter, we'll be able to deliver these treatments to our therapists and adapt our model as needed to be able to make them accessible within the context of our infrastructure. But it might be group. I think that, if that's the model, then there's probably gonna be a lot of group sessions that are gonna come out. So we're already doing a lot of group work, so we're basically set up for all of this. We're set up, even if we're working with people who need to be titrated off their medication, it's a whole complex infrastructure we've already planned for all of that. So we're building towards including more medication and eventually being a hub for collaborative care where all these treatments can be delivered through the collaborative care model.
0:42:42.9 Paul F. Austin: Well, and I was gonna bring it back to these protocols that you've developed. You've developed group protocols, relationship protocols, you've develop protocols for individuals, you've developed... I think you mentioned five or six protocols that you have there. And so I feel like that orientation, it could be right now, 80% of your sessions are individual sessions or 90%, and maybe when psilocybin and MDMA come out, that shifts into being 30% group or 40% group, because that's much more, not even scalable, but just from a financial and accessibility perspective, makes it a lot more easier. What about health insurance? Tell us a little bit about Journey Clinical's relationship with health insurance, how that relates to ketamine-assisted psychotherapy? From what I understand, Spravato, which has been FDA approved is the only ketamine that is covered by health insurance, whereas from what I understand, most of your therapist should be working with a generic ketamine. So how does health insurance come into the play for Journey Clinical specifically in this context?
0:43:52.5 Jonathan Sabbagh: Yeah, that's a great question. So health insurance right now, we're out of network for our medical consultations. However, we do provide superbills for every one of our consultations, so they can be partially covered. Again, it's cheap, it's $250 for an intake and 150 for a follow-up. So it's not a very expensive modality in that way. The ketamine itself cannot be covered because it's off-label. But ketamine is basically free, it's like 70 bucks, I don't know, like a three months supply, and most of that is shipping. So in that context, that's not very expensive. And then on the therapist side, it's pretty interesting because it's important to understand what therapists are doing. They're not doing ketamine-assisted psychotherapy, they're not administering ketamine, they're not doing any kind of medical procedure, they're not evaluating a patient for eligibility of ketamine, we're doing all of that for them. The patient is self-administering the ketamine, they're self-administering the blood pressure cough. So the therapists are only giving a therapy session. And so a therapy session is coded as a therapy session, and that's it. The complication comes when the first sessions are like two hours long.
0:45:02.7 Jonathan Sabbagh: There used to be codes for multiple hours, but I think they were changed recently, but they can code these as therapy sessions because that's what they are. And there's no reason to code them differently if you think of someone who's on suboxone, who's having a therapy session, there's no special code for that, it's a therapy session. And if you think about it even more broadly, any kind of psychiatric medication really alters your consciousness. So SSRIs and benzodiazepine, all these medications alter your consciousness and there's no difference. And so we work very closely with our therapist to make them understand their scope of practice, they're never involved at any part that is linked to prescriptions, to delivery, to outcome monitoring, to eligibility, it's all us. And so we're taking on all of the medical legal risk basically, and the therapists are simply doing a therapy session and that's what's up. So sometimes it can be covered by insurance if they're in network. Right?
0:45:57.7 Paul F. Austin: Yeah, that's helpful. That makes a lot of sense. And of course, when those therapeutic sessions become six hours or seven hours, potentially the MDMA or psilocybin, and that, I think that's where you're saying, we'll have to see what the rules come out, the regulations come on in terms of what actually needs to happen for these, for MDMA and psilocybin potentially.
0:46:14.4 Jonathan Sabbagh: Yeah, I heard that MAPS is working to get a code for MDMA, it's a psychotherapy, so that would be good. I mean, they're gonna have to get this covered by insurance for it to be commercially viable.
0:46:26.2 Paul F. Austin: Yeah, 'cause $15,000 as a treatment is not...
0:46:27.8 Jonathan Sabbagh: It's a lot of money. Yeah.
0:46:27.8 Paul F. Austin: Is not affordable for most folks. So next question, I wanna stay in this decentralized democratized access angle. And what we know in the broader psychedelic space is Oregon has legalized psilocybin, Colorado has kind of legalized all psychedelics, although it's only for personal possession and you can't sell it, sort of this grow-gather-gift model, there is decriminalized access everywhere. And a lot of folks, including myself, believe that this sort of decentralized approach, decriminalization and state-by-state legalization will outpace FDA approval because of all the bureaucracy that's involved with the FDA. We've already seen this in cannabis, right? I think cannabis is still a Schedule I federally illegal substance, whereas it's now legal in I think 20 states and medically available in 40 states, something like that. So I'm just curious, when you consider that from a vision perspective, from a CEO perspective, what do you do with that? Does that matter to you, or are you just explicitly focused on clinicians, FDA approval and things that can happen essentially within the traditional medical system?
0:47:42.1 Jonathan Sabbagh: Yeah, that's a great question. So I think it's wonderful that things are being decriminalized on a state-by-state basis. I think the war on drug doesn't work, so I think that decriminalizing these substances is really good and positive. From our perspective, we chose to operate within a medical model, and so we're gonna work with FDA approval and FDA approved drugs. The reason why we chose to do that is because I think that to enact change at scale, you have to operate within the system, and we exist within the western medical system. And so for us it is to operate within that system, to be able to integrate these treatments at scale nationally as a go-to adjunct to therapy. And so that's why we're working with FDA approved drugs, but it doesn't mean that there are not great things happening in the decrim level on different states that is not great providers. For us, the most sustainable, safe way and scalable way to do it was to work with licensed mental health professionals, FDA approved drugs within a specific treatment modality and expand based on that. And as a company, the market size is very large, and so it's a bit of a different broader play. It doesn't mean that there's not gonna be awesome companies that are gonna work on a state level, just like cannabis and do some really good work.
0:49:08.1 Paul F. Austin: Yeah, you gotta know your focal point right?
0:49:11.0 Jonathan Sabbagh: Yeah.
0:49:11.4 Paul F. Austin: From a strategic perspective, there are things you can do and there are things that you can't do. And when it comes to that more decriminalized model, even with what we're doing at Third Wave, this is what I see as a really great opportunity from an education provider and community network is how do we create much like what you're doing in terms of health tech infrastructure. I would see it as the network for legal psychedelic use to ensure that there're vetted and verified providers, to ensure that it happens within a supportive community. So I feel like there are a lot of other groups that are focused on that, and that I hope there are more and more groups that come out as regulations and as laws start to change around psychedelics. 'Cause it will take an army, it will take massive push and group of people. This is, as you said, the mental health crisis is the biggest health crisis in the world today, and so there's a lot of ground to cover to ensure that people feel more than anything supported. I'll come back to the point that you made that Journey Clinical is not necessarily a psychedelic company. You're creating infrastructure to support healing and mental health, and right now you've landed on ketamine-assisted psychotherapy is an incredibly effective modality to help facilitate that process.
0:50:34.1 Paul F. Austin: And I think that is true generally, that we have to move away from a biological reductionist model and move more into like you said, a collaborative care and model of support that really emphasizes the necessity of human connection for real healing in a way.
0:50:51.3 Jonathan Sabbagh: Yeah, 100%. I think that for our perspective, we wanna take a holistic view on people's mental health and people's health, and so I think that's a direction that the world is trending towards that people want, and that makes more sense than any kind of disjointed, disintegrated approach.
0:51:09.8 Paul F. Austin: Exactly, yeah. Integrating is critical. Okay, CEO question, from one CEO to another CEO. Let's say you have a vision for Journey Clinical, you've raised not an insignificant amount of money from some incredible funds and individuals to support your journey, to support the growth and development of your company, and let's say I gave you a wand or a magic stick or a talking stick. And basically, you said the magic words and Journey Clinical became everything that you ever wanted it to be, it grew into everything that you wanted it to be. Just tell us a little bit about that vision, about that dream. If everything were to go well, if you were to be as successful as you could ever imagine with what you're doing through Journey Clinical, where are we in five years, in 10 years, in 15 years? What does that look like for you?
0:52:11.3 Jonathan Sabbagh: Yeah, I think that we're the main infrastructure... I think we already are the only company in the space that's taken this approach, and so our objective is to become the hub for collaborative care in America. I think really there's a real opportunity for us to do that and we're really working towards that. So that starts with ketamine, it will evolve with MDMA and psilocybin and probably beyond that. So we've got a good roadmap to be able to do that with a really, really strong team. And so we're pretty excited about the future.
0:52:42.9 Paul F. Austin: The hub of collaborative care. I love that. Okay, what do you have coming up in the next, whether from a personal level, from a business level, from a whatever. What are you most excited about in the next three to six to nine months for 2023 in terms of what you're building, what you're creating, what you have going on? Just bring us a little bit into what gets you up in the morning? What makes you excited?
0:53:04.0 Jonathan Sabbagh: Yeah, I mean, we have an awesome team. We actually, as a company, choose to run very lean. So it's been an approach that we've had is that we have a very small team, but we hire highly competent individuals, and so that is good. It's a blessing and a curse because that means that everybody's overworked a little bit, but it's also a type of people that enjoy that work, and so I think we're excited to start hiring a few more people. I think that were one of the few companies in the space that's actually hiring today, and we've been successful doing that for the right kind of people. And so that's a big task on Myriam and mine's desk today is to hire people to come in and plug into the company. We're very excited for the growth ahead, I think we've only scratched the surface of the size of network that we can build going from 30 to 800 in 10 months was great. I think we were able to really, really substantially ramped that up, same with the patients, expanding our protocols, our product. So there's a lot of work for us ahead, we never have not enough work. And I'm very excited about keeping that going. This is the most fun I've had in my life, so I have a lot of fun.
0:54:18.4 Paul F. Austin: Are you burnt out?
0:54:19.5 Jonathan Sabbagh: Yeah, it's been an interesting process, so I definitely felt burnt out at the end of last year when we closed our Series A, and I took the time to rest and when learning, I think as any found there probably goes through is that there are phases where you're doing everything, then there's phases where you start to hire people who can help you. We try to hire people that know more than us. I don't know that much, so I'm really always happy to hire people who are way smarter than me. And they're starting to do, like we get away from the doing as a founder and help with the vision and the directionality. And so I think learning about integrating self-care into that process and accepting that this is a marathon, not a sprint, although there are many sprints in this marathon, I think has been another learning curve for Myriam and I. And so simple things like going back to yoga and taking care of myself and losing some weight and sleeping and taking a vacation or from time to time is equally important as stronger execution.
0:55:23.2 Jonathan Sabbagh: So this is a learning curve. We're in here for a few years, we really love it, and if we wanna last on the long run, we need to learn how to take care of ourselves. So that's been a process for us, but at times, so I've been managing my levels of burnout and learning to recognize when I'm feeling that way. Because it also influences your decision-making in a negative way. All of a sudden, if you're really tired, your decision-making starts to get a little skewed, and so investing in that a little bit has been a real value add for me this year, but we're still very lean, so yeah, we're a little burnt out.
0:56:00.0 Paul F. Austin: I saw a great reframe on LinkedIn from Shane Heath, who founded MUDWTR and it was an article in Business Insider or something like that, and it was about how he really emphasizes performance culture, not necessarily hustle culture. Now, granted, MUDWTR is in LA. It's in Venice, it's a different vibe than New York, obviously, but I think that lens of performance culture allows... I know it's allowed me and allowed our team as well to go, let's take the 10 to 20 year vision rather than the quarterly vision, and let's understand that, yeah, there are things that need to be executed against and milestones that need to be hit. And as you said it's a marathon, not a sprint. We don't wanna burn all of our engines in the first year or two, it's important to have that longevity of everything that we're doing.
0:56:50.2 Jonathan Sabbagh: Yeah, 100%. That really resonates with me, like you have to have... You have the KPIs, you have your quarterly OKRs, you have all this work that you put in place, but down the line, you really need to work towards a greater vision. It's also really important for people in the company to know what they're working towards, what that vision find meaning in that work. So we work a lot on trying to convey that and having people who... And we actually, we did clarity pulse surveys recently, we did a 360 with our team. So we try to understand where we're good, where we're not good, where we're confusing people, where people are feeling confused, and just really make sure that people feel a meaning in their work, and that we are setting everybody up for success, including ourselves. So that's constant work, and it's constant discovery, and it's really psychedelic. Super psychedelics. Yeah, great.
0:57:39.7 Paul F. Austin: Well, Johnathan, thanks for joining this podcast. It's been in a long time in the making. I think ever since we first connected in Miami way back when... I'm glad we finally got to sit down. If there are any clinicians who are listening to this, who are interested in what Journey Clinical is up to and potentially joining your provider network, where can they go? More information, more details, things like that.
0:58:02.2 Jonathan Sabbagh: Yeah, sure, they can go to journeyclinical.com and they can set up an appointment with our team and we'll happily do a demo for them and walk them through the product, and help them get onboarded.
0:58:13.7 Paul F. Austin: Great, well, I love what you're building.
0:58:16.1 Jonathan Sabbagh: Thank you.
0:58:16.8 Paul F. Austin: I think I mentioned this to you from day one, the model is brilliant, that focus on collaborative care and really supporting the entire infrastructure is so necessary and needed, and I find... I think you're striking a really good balance between decentralization and the medical model and finding a way to build a new system from within, which is difficult and challenging, and you've made incredible strides so far in that process. So congratulations on all success so far...
0:58:55.7 Jonathan Sabbagh: Thank you very much.
0:58:55.8 Paul F. Austin: And I wish you all the success in the future for what you're building.
0:59:00.0 Jonathan Sabbagh: Thank you, same to you and thanks for having me on. That was a lot of fun.
[music]
0:59:08.0 Paul F. Austin: Hey, folks, this conversation is bigger than just you or me, so please leave a review or comment so others can find the podcast. This small action matters way more than you can even imagine. You can also go deeper into this episode at thethirdwave.co/podcast, where you'll find full show notes, transcripts, and all the links that were mentioned in this conversation. To get weekly updates from the leading edge of this third wave of psychedelics, sign up for our newsletter at thethirdwave.co/newsletter. You can also find us on Instagram at @thirdwaveishere, or subscribe to our YouTube channel at youtube.com/thethirdwave.